
There aren’t any studies that show people who get root canals have a higher risk of cancer. In fact, research on the link between cancer and endodontic procedures like root canals shows that people who have had these treatments have a lower risk of certain cancers.
The danger of these claims is that these fears can crowd out other real cancer risks or health concerns. Viewers may focus on previously completed root canals while ignoring well known risk factors for cancer or infection, including smoking, weight gain, and failing to get the right cancer screening tests on time. To be blunt, even if there is some truth to this whole idea, your old root canal is probably not harming your body nearly as much as your bleeding gums, cigarette smoking, or undiagnosed sleep disorder. Illness is cumulative, so it’s important to focus on the bigger concerns first when working towards optimal health and well-being.
HOWEVER, there is one very important thing that the documentary ROOT CAUSE gets right! There are many patients walking around with active infection in their tooth roots and bone who have ABSOLUTELY NO IDEA that there is any problem whatsoever. We know this is true because we have advanced 3D imaging that allows us to routinely see infections in the tooth and bone that simply cannot be seen in traditional dental X-rays and are asymptomatic.
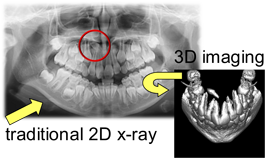
Because of this, we have been able to help countless patients get rid of active infection in their body quickly and easily. The first step to health is accurate and actionable diagnosis!
In looking at documentaries and other health related information on the internet, it’s important to remember a phrase we often share with our patients:
“Everything on the internet is somewhat right for some people.”
BOTTOM LINE: The most important thing is that you find a provider that you trust who will help you navigate through all the conflicting information out there, and who will have an in depth understanding of your individual circumstances in order to provide you customized advice on how to get and stay healthy.
While root canals can’t save every tooth, leaving the natural tooth intact helps maintain the jawbone’s original structure. Without the original tooth, the surrounding jawbone that once supported it will eventually break down, affecting a person’s appearance and their ability to chew.





 Our patients often ask us about oil pulling, or ‘swishing’: it’s an alternative treatment purported to rid your body of unwanted bacteria through the process of swishing vegetable oil (mostly coconut oil) around your mouth. Those who swear by the process claim that it whitens teeth, fights bad breath, and gets rid of bacteria stuck in hard to reach places.
We totally support alternative wellness, even when it comes to your teeth. Understand that oil pulling may sound like a great alternative oral care solution, but it can never replace brushing and flossing. Here's some real talk about oil pulling and how we think it can be beneficial:
What is oil pulling?
The process of oil pulling involves putting a tablespoon of liquid vegetable oil, often coconut oil, into your mouth and swishing it around for 20 minutes before spitting it out and brushing it away with a toothbrush and toothpaste. The process gets its name partly from the pushing and pulling of the oil through teeth and mouth, and partly from the way the oil is supposed to pull icky stuff out of your mouth tissues.
The longer you push and pull the oil through your mouth, the more microbes are pulled free. The oil needs to be swished around long enough for it to turn a milky white, which indicates that the bacteria has been "pulled" off. After roughly 20 minutes the solution is filled with bacteria, viruses and other organisms; at this point, the person spits out the oil and rinses thoroughly with water.
How does oil pulling work?
The number of bacteria found in our mouths is usually between 1,000 and 10,000 on each individual tooth. It may sound like a lot, but these guys are tiny! Each of these bacteria have a fatty outer coating, and when they come into contact with another fatty substance, such as oil, they have a tendency to stick to that substance. Since liquid oil has the ability to get into hard to reach areas of the mouth that a toothbrush would miss, it is thought to be able to pick up bacteria that may have otherwise stayed hidden.
People that “oil pull” state that it has helped whiten their teeth, alleviate halitosis, and even reduce gingivitis. In many cases, people also claim that it helps “prevent” cavities, as well as relieve gum and tooth sensitivity.
What we believe
There is clear evidence that many diseases and conditions are influenced by the mouth’s ecology and bacteria, and we understand the topic of oil pulling is valid when patients wonder why oil pulling has been encouraged by dental professionals as a supplemental therapy for patients, especially if we are in the business of “preventing” oral health problems.
We support holistic approaches to your oral care. You just have to be smart about it and consider your individual dental health: there are certain types of infections that oil pulling will not resolve, and you have to be aggressive about treating those. It won’t take away raging gum infections or cavities. Oil pulling may remove bacteria, but it doesn't kill bacteria, and that's a big difference.
BOTTOM LINE
If oil pulling is used alone, without regular brushing and flossing, then no, it is not an effective way to keep your mouth healthy. It will not heal existing decay. However, when used in conjunction with proper daily brushing and flossing habits as a preventive measure, it may improve bad breath, help to decrease staining, and benefit in other ways. If you have dry mouth issues, we absolutely believe pre-bedtime oil pulling can be helpful.
Our patients often ask us about oil pulling, or ‘swishing’: it’s an alternative treatment purported to rid your body of unwanted bacteria through the process of swishing vegetable oil (mostly coconut oil) around your mouth. Those who swear by the process claim that it whitens teeth, fights bad breath, and gets rid of bacteria stuck in hard to reach places.
We totally support alternative wellness, even when it comes to your teeth. Understand that oil pulling may sound like a great alternative oral care solution, but it can never replace brushing and flossing. Here's some real talk about oil pulling and how we think it can be beneficial:
What is oil pulling?
The process of oil pulling involves putting a tablespoon of liquid vegetable oil, often coconut oil, into your mouth and swishing it around for 20 minutes before spitting it out and brushing it away with a toothbrush and toothpaste. The process gets its name partly from the pushing and pulling of the oil through teeth and mouth, and partly from the way the oil is supposed to pull icky stuff out of your mouth tissues.
The longer you push and pull the oil through your mouth, the more microbes are pulled free. The oil needs to be swished around long enough for it to turn a milky white, which indicates that the bacteria has been "pulled" off. After roughly 20 minutes the solution is filled with bacteria, viruses and other organisms; at this point, the person spits out the oil and rinses thoroughly with water.
How does oil pulling work?
The number of bacteria found in our mouths is usually between 1,000 and 10,000 on each individual tooth. It may sound like a lot, but these guys are tiny! Each of these bacteria have a fatty outer coating, and when they come into contact with another fatty substance, such as oil, they have a tendency to stick to that substance. Since liquid oil has the ability to get into hard to reach areas of the mouth that a toothbrush would miss, it is thought to be able to pick up bacteria that may have otherwise stayed hidden.
People that “oil pull” state that it has helped whiten their teeth, alleviate halitosis, and even reduce gingivitis. In many cases, people also claim that it helps “prevent” cavities, as well as relieve gum and tooth sensitivity.
What we believe
There is clear evidence that many diseases and conditions are influenced by the mouth’s ecology and bacteria, and we understand the topic of oil pulling is valid when patients wonder why oil pulling has been encouraged by dental professionals as a supplemental therapy for patients, especially if we are in the business of “preventing” oral health problems.
We support holistic approaches to your oral care. You just have to be smart about it and consider your individual dental health: there are certain types of infections that oil pulling will not resolve, and you have to be aggressive about treating those. It won’t take away raging gum infections or cavities. Oil pulling may remove bacteria, but it doesn't kill bacteria, and that's a big difference.
BOTTOM LINE
If oil pulling is used alone, without regular brushing and flossing, then no, it is not an effective way to keep your mouth healthy. It will not heal existing decay. However, when used in conjunction with proper daily brushing and flossing habits as a preventive measure, it may improve bad breath, help to decrease staining, and benefit in other ways. If you have dry mouth issues, we absolutely believe pre-bedtime oil pulling can be helpful.
 Whether it's echinacea or aspirin, always tell your dentist about any medications and supplements you are taking.
Everything you ingest, even vitamins, causes a certain reaction. If your dentist doesn’t know what drugs or supplements you have taken, he or she will not know how to protect you from possible substance interactions. This is particularly important if you are undergoing any surgical treatment.
Conventional versus herbal
Although many conventional (prescription and over-the-counter) medications sold in the United States are derived from plants, they are different from herbal medications. Conventional drugs, which must be approved for use by the Food and Drug Administration, are based on an active ingredient or chemical that manufacturers synthesize when they develop the drug. In other words, a conventional drug is based on a chemical that is made in a laboratory, even though it may have originally come from a plant.
Herbal (also called botanical or alternative) medications are made from natural chemicals extracted from a plant and are produced either in original form (sometimes combined with other herbal extracts) or refined. When an herbal medication is refined, the essential extract is taken out of the plant source, concentrated and then added back to make the original herbal medication more potent.
Combinations to avoid
Even seemingly innocuous herbal and vitamin supplements can have serious side effects for a few dental patients. Here are some combinations to be aware of:
Ginkgo biloba and vitamin E can be dangerous when taken with aspirin because they each can act as blood thinners. The combination may cause difficulties in blood clotting, which could be serious for patients undergoing surgery.
Taking high dosages of vitamins before undergoing anesthesia can also cause concern. In particular, vitamin C, often taken in high dosages for cancer treatment, can weaken the efficiency of anesthesia, among other problems.
Calming supplements, such as Kava Kava or St. John's Wort, can strengthen the effects of anesthesia.
What your dentist can do
Always provide your dentist with a complete medical history, including any herbal medication and conventional drugs you are taking.
Some patients who take alternative medicines are afraid the dentist will not respect their decision to take an herbal medication and will tell them to stop taking it; however, as herbal medications become more popular, many dentists are beginning to use them in their practices. Your dentist might even have an alternative, herbal solution for you.
If an herbal medication could interfere with your dental treatment, your dentist may ask you to stop taking the medication until the treatment is complete. The dentist also may be able to prescribe a different drug for treatment, if one is available.
More:
Whether it's echinacea or aspirin, always tell your dentist about any medications and supplements you are taking.
Everything you ingest, even vitamins, causes a certain reaction. If your dentist doesn’t know what drugs or supplements you have taken, he or she will not know how to protect you from possible substance interactions. This is particularly important if you are undergoing any surgical treatment.
Conventional versus herbal
Although many conventional (prescription and over-the-counter) medications sold in the United States are derived from plants, they are different from herbal medications. Conventional drugs, which must be approved for use by the Food and Drug Administration, are based on an active ingredient or chemical that manufacturers synthesize when they develop the drug. In other words, a conventional drug is based on a chemical that is made in a laboratory, even though it may have originally come from a plant.
Herbal (also called botanical or alternative) medications are made from natural chemicals extracted from a plant and are produced either in original form (sometimes combined with other herbal extracts) or refined. When an herbal medication is refined, the essential extract is taken out of the plant source, concentrated and then added back to make the original herbal medication more potent.
Combinations to avoid
Even seemingly innocuous herbal and vitamin supplements can have serious side effects for a few dental patients. Here are some combinations to be aware of:
Ginkgo biloba and vitamin E can be dangerous when taken with aspirin because they each can act as blood thinners. The combination may cause difficulties in blood clotting, which could be serious for patients undergoing surgery.
Taking high dosages of vitamins before undergoing anesthesia can also cause concern. In particular, vitamin C, often taken in high dosages for cancer treatment, can weaken the efficiency of anesthesia, among other problems.
Calming supplements, such as Kava Kava or St. John's Wort, can strengthen the effects of anesthesia.
What your dentist can do
Always provide your dentist with a complete medical history, including any herbal medication and conventional drugs you are taking.
Some patients who take alternative medicines are afraid the dentist will not respect their decision to take an herbal medication and will tell them to stop taking it; however, as herbal medications become more popular, many dentists are beginning to use them in their practices. Your dentist might even have an alternative, herbal solution for you.
If an herbal medication could interfere with your dental treatment, your dentist may ask you to stop taking the medication until the treatment is complete. The dentist also may be able to prescribe a different drug for treatment, if one is available.
More:  No doubt eco-friendly has become an important ‘buzz phrase’ in most dental offices, not only because it is the right thing to do, but also because of patient awareness and inquiries. Still not sure what that means for your smile? Let these trends fill you in.
The paper factor: This past summer, the American Dental Association endorsed new deadlines for dental offices to have devices that capture dental amalgam waste so that it can be recycled. More and more dental offices are thinking and acting ‘green’ by reducing the amount of plastic used in multiple areas such as substituting digital scanning instead of plastic impression trays, and substituting cloth and paper for plastic in both sterilization and other patient protection disciplines.
Digital do-good: Digital is quickly replacing paper and plastic, so much so that many offices have converted to all-digital—especially in X-rays, charting and photo records. And while it doesn’t necessarily affect the health of a patient, it is something that helps the greater good. Biodegradable cleaners and disinfectants are now ‘in’ and dentists have become conscious of how they can make a difference in their offices every day to make their contribution towards cleaner living for our planet. We also now have 3D imaging, which is the most accurate way to get impressions, and we can use it for crowns, veneers and Invisalign. No more 'goop' is needed to get a mold of your teeth.
Lasers get more love: Sure, lasers sound like a high-tech solution for just about anything, but there’s also a real impact on what they help in terms of the environment. By use of a laser and air-abrasion, we can avoid removing so much less of a patient’s tooth structure was removed, and all without any local anesthetic. This is the future of dental patient care, which means fewer materials used because the restorative surface is so much smaller. And because many of the dental materials used today are resin-based, less material used means less resin. Also, keeping restorations smaller means less water used.
Metal is minimized: According to New York cosmetic dentist
No doubt eco-friendly has become an important ‘buzz phrase’ in most dental offices, not only because it is the right thing to do, but also because of patient awareness and inquiries. Still not sure what that means for your smile? Let these trends fill you in.
The paper factor: This past summer, the American Dental Association endorsed new deadlines for dental offices to have devices that capture dental amalgam waste so that it can be recycled. More and more dental offices are thinking and acting ‘green’ by reducing the amount of plastic used in multiple areas such as substituting digital scanning instead of plastic impression trays, and substituting cloth and paper for plastic in both sterilization and other patient protection disciplines.
Digital do-good: Digital is quickly replacing paper and plastic, so much so that many offices have converted to all-digital—especially in X-rays, charting and photo records. And while it doesn’t necessarily affect the health of a patient, it is something that helps the greater good. Biodegradable cleaners and disinfectants are now ‘in’ and dentists have become conscious of how they can make a difference in their offices every day to make their contribution towards cleaner living for our planet. We also now have 3D imaging, which is the most accurate way to get impressions, and we can use it for crowns, veneers and Invisalign. No more 'goop' is needed to get a mold of your teeth.
Lasers get more love: Sure, lasers sound like a high-tech solution for just about anything, but there’s also a real impact on what they help in terms of the environment. By use of a laser and air-abrasion, we can avoid removing so much less of a patient’s tooth structure was removed, and all without any local anesthetic. This is the future of dental patient care, which means fewer materials used because the restorative surface is so much smaller. And because many of the dental materials used today are resin-based, less material used means less resin. Also, keeping restorations smaller means less water used.
Metal is minimized: According to New York cosmetic dentist  Having chronic gum disease gives people a 70% increased risk of developing Alzheimer's, scientists have found.
Research has linked gum problems and dementia for several years. These studies have usually been small in which a snapshot of people's health in time has been taken, rather than large studies tracking their likelihood of developing disease in the long term.
One of the largest longitudinal studies on the topic has now found a strong correlation between gum disease, or periodontitis, and risk of Alzheimer's. The
Having chronic gum disease gives people a 70% increased risk of developing Alzheimer's, scientists have found.
Research has linked gum problems and dementia for several years. These studies have usually been small in which a snapshot of people's health in time has been taken, rather than large studies tracking their likelihood of developing disease in the long term.
One of the largest longitudinal studies on the topic has now found a strong correlation between gum disease, or periodontitis, and risk of Alzheimer's. The  Stress can do a lot of bad things to your body, from headaches to backaches, high blood pressure to heart disease. But can
Stress can do a lot of bad things to your body, from headaches to backaches, high blood pressure to heart disease. But can  Gingivitis is one of the
Gingivitis is one of the