
Our dental patients should know why we are listening (and looking) closer for the telltale signs that they may not be sleeping well.
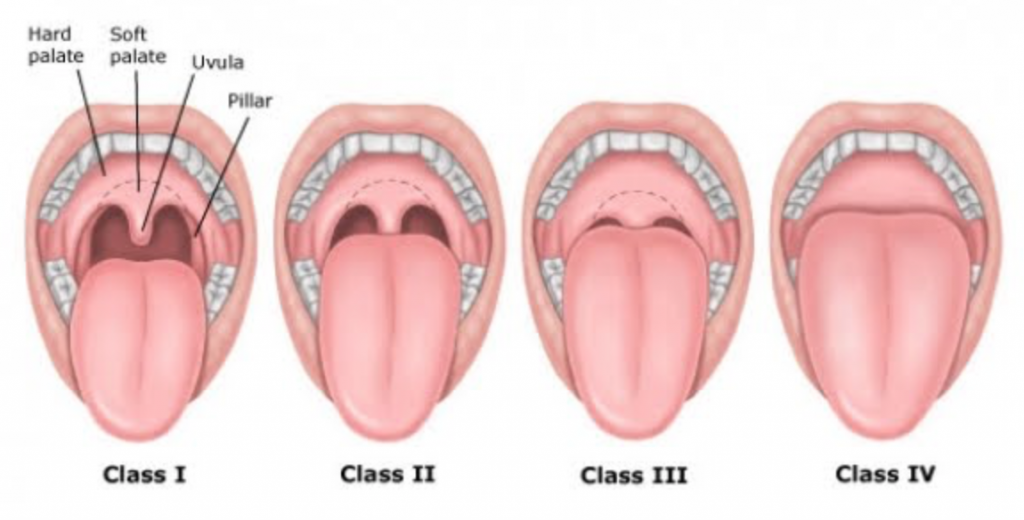
It’s a typical day on the job: we see several patients, observe and clean their teeth and get them ready to see Dr. Clark. As we're cleaning one patient’s mouth, something seems a little off. We notice that they have a smaller mouth and a normal size tongue, and it’s difficult to see past their soft palate as they say “Ahhhh.” When we ask the patient about their week, they complain that they’ve been feeling tired and haven’t been sleeping well at night. We've experienced patients with a similar story and appearance before. What’s the connection?
Research shows that 24.1% of patients are more likely to visit their dentist than their physician for an annual exam, which places a responsibility on us to be knowledgeable about the oral signs that may be indicative of a larger health condition.

Obstructive sleep apnea (OSA) is a common disorder that affects 20-30% of adults. It is also the most common undiagnosed sleep disorder and chronic disease in Western society, with up to 80 percent of people that suffer from moderate to severe OSA unaware of their condition.
This is important considering untreated OSA can take up to 20 years off of your lifespan. It ages your body, wreaks havoc on your immune and cardiovascular system, and dramatically decreases quality of life.
OSA sufferers often experience an inability to concentrate or focus on everyday tasks because they experience repeated microarousals, which eliminate the opportunity to have complete restorative sleep cycles. They also can experience morning headaches, clenching and grinding, and dry mouth, which can have a severe negative impact on dental health and overall wellness.
Additionally, the disorder is linked to a number of comorbidities, including cardiovascular disease, type 2 diabetes, stroke and even Alzheimer’s. Those that suffer from OSA are two times more likely to get into a car wreck, as sleep apnea causes a decrease in cognitive functioning.
Sleep apnea can originate in the throat, which makes us the front line in detection of the physical signs that a patient may suffer from if they have OSA. Many patients with sleep apnea DO NOT experience the tell tale symptoms they have heard about; snoring, daytime fatigue, witnessed cessations of breathing during sleep, high blood pressure, and waking from sleep with a gasp or choking sound. Instead of focusing only on these subjective symptoms, the easiest way to gauge risk of obstructive sleep apnea is to look in the mouth…
What we look for: signs and symptoms
Patients with OSA display many symptoms that can be observed simply by looking into the mouth. The MOST predictive signs include:
- Small or recessed chin
- Scalloped tongue
- Eroded enamel / Clenching and Grinding
- Mallampati Classification of III or IV
Other signs we assess that are correlated with OSA include:
- High BMI
- Morning Headaches
- Narrow Arch or Small Mouth
If any of these signs are observed, or we note other symptoms that may be indicative of sleep apnea (for example, if the patient is obese or complains of a dry mouth), we often ask follow-up questions, including:
- Do you snore?
- Do you wake during the night for any reason? Is it 4 hours into your sleep cycle?
- Do you feel well rested after getting a full night of sleep?
Patients who confirm these symptoms should be further assessed. Dentists and dental hygienists can use screening tools for early detection of risk factors. If, after screening, we believe that a patient displays signs of sleep apnea, it is our responsibility to educate our patient and provide them the support they need to get tested.
OSA is not just overweight or older people who snore loudly, it's young otherwise healthy people who just have too much soft tissue (tongue, tonsils, soft palate) in the throat.
Each Downtown Dental patient (as well as those referred to Downtown Dental by their medical doctors) are provided with a sleep consultation appointment to discuss all the risks, and benefits associated with proper treatment of OSA. Based on the medical doctor recommendation along with our own assessments, we will follow the best approach to a customized, comprehensive treatment plan with ongoing care.


 DD Team Members experience the advanced TMJD course with an emphasis in posture, dental orthopedics and upper cervical health in relation the the TMJ.[/caption]
DD Team Members experience the advanced TMJD course with an emphasis in posture, dental orthopedics and upper cervical health in relation the the TMJ.[/caption]
