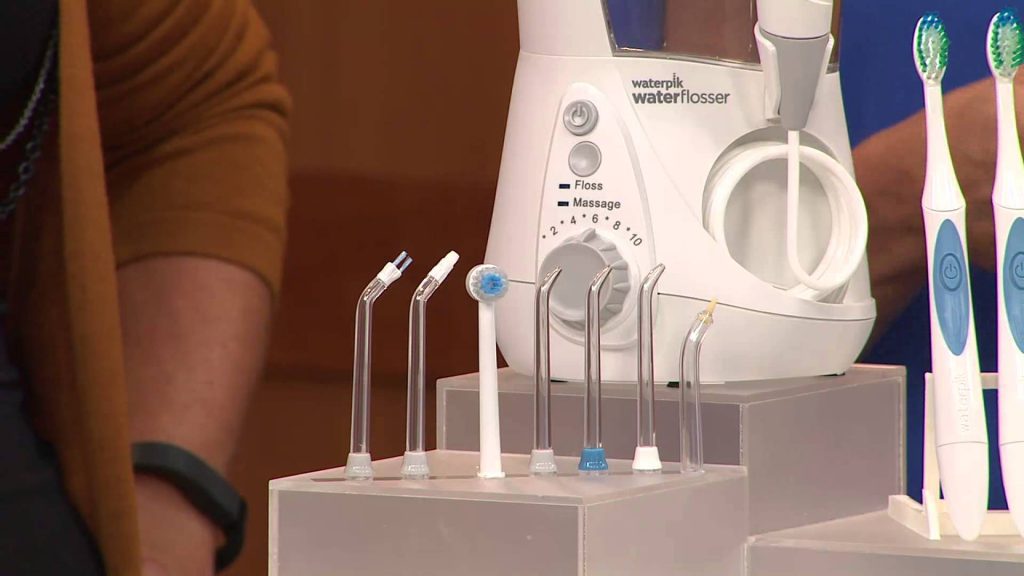
You have a choice of more than just dental floss to clean between your teeth. There are now hundreds of products on the market for interdental cleaning, ranging from wooden sticks to interdental brushes, and now even oral irrigation devices also known as water flossers (or Water Piks.)
Clinical studies of the Water Pik have found that the water flosser is 51% more effective for reducing gingivitis, twice as effective at reducing gingival bleeding, and 29% more effective at removing plaque. The Waterpik can give you healthier teeth and gums when being used for just a minute per day.
What is a Water Flosser or Water Pik?
A water flosser is an oral health appliance designed for dental care at home: consider it a 'power washer' for your gums.
Although sizes and features vary, all water flossers include:
- Motor with pump
- Water reservoir
- Special tips for specific cleaning needs
The motor and pump cause a stream of pressurized, pulsating water to flow from the reservoir through the tip and into the mouth.
The targeted stream of water removes plaque, food particles, and bacteria in a way that’s more effective, more comfortable, and easier than traditional string floss. The pulsating action also stimulates gum tissue for added health benefits.
Why Choose a Water Flosser?
If you don’t like string floss, don’t floss often, or find string floss hard to use, a water flosser can be the answer.
- Many people find water flossing easier and more pleasant than using string floss, and they may floss more often as a result.
- Gum disease prevention and treatment is another reason to use a water flosser. Waterpik®Water Flossers are clinically proven to reduce gingivitis, remove plaque, and improve gum health.
- Water flossers are especially useful for cleaning braces and other orthodontics, as well as cleaning bridges, crowns, and dental implants.
- Water flossers are helpful for people with dexterity issues, such as arthritis, who find string flossing difficult.
What About Toothbrushing?
For daily home care, we recommend:
- Brushing your teeth 2x a day for 2 minutes
- Flossing once a day to clean between your teeth
Although water flossing reaches areas that tooth brushing can’t, it is not a replacement for brushing your teeth. Rather, it is an alternative to string floss, interdental brushes, or floss threaders to remove plaque and debris that brushing leaves behind. There will also be some patients for whom we recommend using regular dental floss in addition to water flossing, but we like to see every patient using a Water Pik, if possible.
Is Water Flossing Messy?
Compared to string floss, water flossing is easier and doesn't require you to put your hands in your mouth or deal with used string floss.
The correct technique is they key. Unlike string floss, you don’t need to look in the mirror or hold your mouth open wide.
To use a water flosser, place the flosser tip in your mouth, close your lips most of the way, and lean over the sink. Then turn the power on. As you floss along the gumline and between your teeth, allow the water to empty from your mouth into the sink.
Essential takeaway: flossing is designed to prevent bacterial changes that lead to gum disease. Gum disease has been linked to heart conditions, diabetes, and infection. If regular flossing isn't getting the results you're looking for, a water flosser might be the best option for you. Let's talk about this during your next appointment.



 Though the link between dental health and heart health is not completely clear, experts say it’s important to take care of both.
Claiming around 610,000 lives each year, heart disease is the No. 1 killer of both men and women in the U.S.1 Did you know that research has found a link between this deadly disease and the health of your gums?
Having gum disease increases the risk of a first heart attack by 28%, according to a 2016 study by the Karolinska University Hospital in Sweden.2
“Although the findings indicate a strong link between gum disease and heart disease, it’s still unclear whether one actually causes the other,” says the American Heart Association. The two conditions have some of the same risk factors, including smoking, poor nutrition and diabetes. Researchers believe that inflammation caused by periodontal disease may be responsible for the connection.3
Though the link between dental health and heart health is not completely clear, experts say it’s important to take care of both.
Claiming around 610,000 lives each year, heart disease is the No. 1 killer of both men and women in the U.S.1 Did you know that research has found a link between this deadly disease and the health of your gums?
Having gum disease increases the risk of a first heart attack by 28%, according to a 2016 study by the Karolinska University Hospital in Sweden.2
“Although the findings indicate a strong link between gum disease and heart disease, it’s still unclear whether one actually causes the other,” says the American Heart Association. The two conditions have some of the same risk factors, including smoking, poor nutrition and diabetes. Researchers believe that inflammation caused by periodontal disease may be responsible for the connection.3

 Photo credit: Dreamstime.com[/caption]
A lot of people believe that they have already fully comprehend what osteoporosis is all about and what they can do to either prevent or cure the condition. Osteoporosis refers to a disease characterized by extremely fragile and less dense bones. The main causes of the problem are aging, menopause, and lack of Vitamin D and calcium.
Recent advancements in research have shed new light on the entire condition, showing clear reasons for its existence and what sufferers can do to treat it. Osteoporosis is a condition worth worrying about because there are predictions that state its ability to affect more than half of the people in America who will be older than age 50 by the year 2020. New research and studies show more relevant information from the process of diagnosing osteoporosis, to preventing and treating it.
Bone health, osteoporosis, and calcium intake
In the past few years, there are a few studies that report conflicting findings about the effectiveness of calcium supplements mainly utilized for prevention of fractures and improvement in bone health. The reason behind this is that there are also findings that show the ability of these supplements to increase a person's risk of suffering from heart diseases and attacks.
According to Douglas C. Bauer, a professor of epidemiology, biostatistics, and medicine, osteoporosis is a result of the lack of calcium consumption, and it has become a common disease among people in the U.S. He further added that it greatly affects the elderly, especially if their intake of calcium is less than their required daily dosage. However, he also stated that it is necessary to follow a high-calcium diet instead of relying on supplements.
The reason behind such a recommendation is that calcium supplements also carry a few adverse side effects. Among the common side effects are minor constipation, increased risk of developing kidney stones, and indigestion. Recent studies also show that calcium supplements increase one's chances of a heart attack. In fact, a nonrandomized study conducted by JAMA’s Internal Medicine just this year figured out that more than 11,000 deaths related to cardiovascular diseases are connected to the increased and continued intake of calcium supplements.
This is the main reason why a lot of experts recommend increasing calcium intake through foods rich in calcium. Choose to eat dairy products with high calcium content, instead of instantly taking the supplement. Food products fortified with extra calcium such as broccoli and kale can also help. If the intake of calcium supplement cannot be prevented, then it is best to discuss the decision with your doctor. This can help in figuring out if there are any complications to this move.
Osteoporosis and its effects on oral and dental health
Osteoporosis is a health condition that greatly affects the bones, since the disease weakens them and makes them capable of breaking easily. Note that aside from negatively hampering overall health and well being, osteoporosis also has a direct relationship on oral and dental health. One should realize that the disease can hamper or damage jawbones. It also triggers dental and oral health issues, including gum or periodontal diseases and loss of teeth.
The dental and oral effects of osteoporosis tend to affect more women than man. This holds true for women who are already on their menopausal phase, unless they regularly use a therapy designed to replace lost hormones and balance them. It should also be noted that even if someone has no teeth and does not wear dentures, the effects of osteoporosis can still affect dental and oral health. Bone weakness and loss may also affect the body ridges that hold dentures in the proper position, resulting in poor-fitting dentures. Studies also show that sufferers of the disease are at risk of requiring new dentures more often than those who have strong, healthy bones.
Osteoporosis has a major impact on the part of the jawbone supporting the teeth. Studies show that a loss in this bone is most likely to cause tooth loss or mobility. Female sufferers of osteoporosis also have a higher likelihood of experiencing tooth loss or mobility than nonsufferers. Low bone density in the jaw triggered by osteoporosis can also lead to other dental issues. For instance, women suffering from osteoporosis are most likely to experience difficulties linked to ill-fitting or loose dentures. The results of various oral and dental surgical procedures are also less than desirable for these women.
The best way to handle this problem is to avoid delaying or postponing dental treatments. Regular dental visits are essential in correcting problems in oral and dental health caused by weak bones. A healthy lifestyle is necessary in strengthening and maintaining good bone health.
Effective tips in optimizing bone health include eating a well-balanced diet, containing high amounts of Vitamin D and calcium, and performing regular physical activities. The best exercises that are beneficial in strengthening bones are jogging, weight training, dancing, and walking.
Another tip is to avoid excessive smoking and alcohol consumption. Remind your patients to immediately report problems to your dental office related to receding or detached gums, ill-fitting or loose dentures, and loose teeth.
Osteoporosis and the life span of women
Based on new reports and studies, especially the ones published and reported by the International Osteoporosis Foundation, women live longer life spans than male sufferers. However, the quality of living of these women will be seriously and adversely affected if they do not take necessary action to protect their bone health. Studies show the vulnerability of postmenopausal women to bone fractures and osteoporosis. Currently, about 200 million women suffer from osteoporosis. Estimates and studies prove that at least one in every three women who are older than 50 will deal with bone fractures due to osteoporosis.
Solutions linked to preventing and managing fracture and osteoporosis are now introduced to women, especially postmenopausal ones. The reason behind this is that women who are older than 50 and serve as breadwinners of their family or caregivers of society need to prioritize the improvement of their bone health. It would be impossible for these women to continue in their roles if their bones were not in good condition.
Researchers also emphasize the need to do a few things that are valuable in preventing the disease as early as possible. It is crucial to take all the necessary actions designed to boost bone health upon reaching menopause. Note that menopause is a critical stage to perform preventive techniques and measures that fight muscle weakness and bone loss leading to falls, fracture, and osteoporosis.
Menopause is also the stage when the resorption of bones exceeds their formation. This triggers the immediate decline in bone mass, further leading to increased bone loss and triggering osteoporosis. This disease can cause bones to become weak and porous. It also increases the vulnerability of bones to fractures. Encourage your patients to take action to strengthen their bones, increase their intake of calcium-rich foods, and regularly visit a specialist to have their bone structure checked to ensure that this will never be a threat to their health and quality of life.
Photo credit: Dreamstime.com[/caption]
A lot of people believe that they have already fully comprehend what osteoporosis is all about and what they can do to either prevent or cure the condition. Osteoporosis refers to a disease characterized by extremely fragile and less dense bones. The main causes of the problem are aging, menopause, and lack of Vitamin D and calcium.
Recent advancements in research have shed new light on the entire condition, showing clear reasons for its existence and what sufferers can do to treat it. Osteoporosis is a condition worth worrying about because there are predictions that state its ability to affect more than half of the people in America who will be older than age 50 by the year 2020. New research and studies show more relevant information from the process of diagnosing osteoporosis, to preventing and treating it.
Bone health, osteoporosis, and calcium intake
In the past few years, there are a few studies that report conflicting findings about the effectiveness of calcium supplements mainly utilized for prevention of fractures and improvement in bone health. The reason behind this is that there are also findings that show the ability of these supplements to increase a person's risk of suffering from heart diseases and attacks.
According to Douglas C. Bauer, a professor of epidemiology, biostatistics, and medicine, osteoporosis is a result of the lack of calcium consumption, and it has become a common disease among people in the U.S. He further added that it greatly affects the elderly, especially if their intake of calcium is less than their required daily dosage. However, he also stated that it is necessary to follow a high-calcium diet instead of relying on supplements.
The reason behind such a recommendation is that calcium supplements also carry a few adverse side effects. Among the common side effects are minor constipation, increased risk of developing kidney stones, and indigestion. Recent studies also show that calcium supplements increase one's chances of a heart attack. In fact, a nonrandomized study conducted by JAMA’s Internal Medicine just this year figured out that more than 11,000 deaths related to cardiovascular diseases are connected to the increased and continued intake of calcium supplements.
This is the main reason why a lot of experts recommend increasing calcium intake through foods rich in calcium. Choose to eat dairy products with high calcium content, instead of instantly taking the supplement. Food products fortified with extra calcium such as broccoli and kale can also help. If the intake of calcium supplement cannot be prevented, then it is best to discuss the decision with your doctor. This can help in figuring out if there are any complications to this move.
Osteoporosis and its effects on oral and dental health
Osteoporosis is a health condition that greatly affects the bones, since the disease weakens them and makes them capable of breaking easily. Note that aside from negatively hampering overall health and well being, osteoporosis also has a direct relationship on oral and dental health. One should realize that the disease can hamper or damage jawbones. It also triggers dental and oral health issues, including gum or periodontal diseases and loss of teeth.
The dental and oral effects of osteoporosis tend to affect more women than man. This holds true for women who are already on their menopausal phase, unless they regularly use a therapy designed to replace lost hormones and balance them. It should also be noted that even if someone has no teeth and does not wear dentures, the effects of osteoporosis can still affect dental and oral health. Bone weakness and loss may also affect the body ridges that hold dentures in the proper position, resulting in poor-fitting dentures. Studies also show that sufferers of the disease are at risk of requiring new dentures more often than those who have strong, healthy bones.
Osteoporosis has a major impact on the part of the jawbone supporting the teeth. Studies show that a loss in this bone is most likely to cause tooth loss or mobility. Female sufferers of osteoporosis also have a higher likelihood of experiencing tooth loss or mobility than nonsufferers. Low bone density in the jaw triggered by osteoporosis can also lead to other dental issues. For instance, women suffering from osteoporosis are most likely to experience difficulties linked to ill-fitting or loose dentures. The results of various oral and dental surgical procedures are also less than desirable for these women.
The best way to handle this problem is to avoid delaying or postponing dental treatments. Regular dental visits are essential in correcting problems in oral and dental health caused by weak bones. A healthy lifestyle is necessary in strengthening and maintaining good bone health.
Effective tips in optimizing bone health include eating a well-balanced diet, containing high amounts of Vitamin D and calcium, and performing regular physical activities. The best exercises that are beneficial in strengthening bones are jogging, weight training, dancing, and walking.
Another tip is to avoid excessive smoking and alcohol consumption. Remind your patients to immediately report problems to your dental office related to receding or detached gums, ill-fitting or loose dentures, and loose teeth.
Osteoporosis and the life span of women
Based on new reports and studies, especially the ones published and reported by the International Osteoporosis Foundation, women live longer life spans than male sufferers. However, the quality of living of these women will be seriously and adversely affected if they do not take necessary action to protect their bone health. Studies show the vulnerability of postmenopausal women to bone fractures and osteoporosis. Currently, about 200 million women suffer from osteoporosis. Estimates and studies prove that at least one in every three women who are older than 50 will deal with bone fractures due to osteoporosis.
Solutions linked to preventing and managing fracture and osteoporosis are now introduced to women, especially postmenopausal ones. The reason behind this is that women who are older than 50 and serve as breadwinners of their family or caregivers of society need to prioritize the improvement of their bone health. It would be impossible for these women to continue in their roles if their bones were not in good condition.
Researchers also emphasize the need to do a few things that are valuable in preventing the disease as early as possible. It is crucial to take all the necessary actions designed to boost bone health upon reaching menopause. Note that menopause is a critical stage to perform preventive techniques and measures that fight muscle weakness and bone loss leading to falls, fracture, and osteoporosis.
Menopause is also the stage when the resorption of bones exceeds their formation. This triggers the immediate decline in bone mass, further leading to increased bone loss and triggering osteoporosis. This disease can cause bones to become weak and porous. It also increases the vulnerability of bones to fractures. Encourage your patients to take action to strengthen their bones, increase their intake of calcium-rich foods, and regularly visit a specialist to have their bone structure checked to ensure that this will never be a threat to their health and quality of life.