Emerging research has suggested a there’s a connection between gum disease and SARS-CoV-2, according to a new report, “The Mouth COVID Connection (MCC).” The study, which has been accepted for publication for the October 2020 issue of the Journal of the California Dental Association (JCDA), found that hospitalized coronavirus patients with prior underlying gum disease are more likely to suffer respiratory failure.
The MCC study found a link between the bacteria produced by swollen, red, bleeding gums, and bone loss—symptoms of chronic periodontitis—and COVID-19. Researchers found that patients with high levels of IL-6 (interleukin), a harmful protein produced by gum disease, were at significantly greater risk of suffering life-threatening respiratory problems. A similar study in Germany tested COVID-19 patients for the IL-6 protein while they were hospitalized and determined that these patients were in critical condition and needed a ventilator to breathe. [caption id="attachment_3940" align="alignright" width="442"]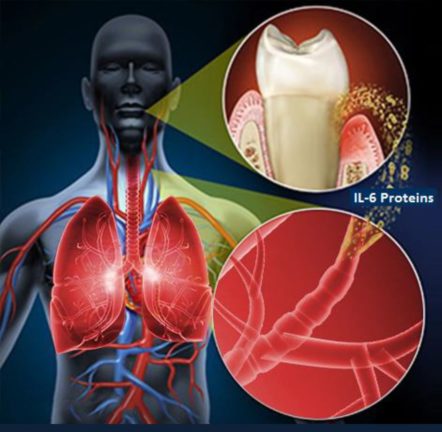 Image: DentalProductsReport.com[/caption]
The study was conducted over a 3-month period by Dr. Shervin Molayem, a dental surgeon based in Los Angeles and founder of the UCLA Dental Research Journal, and Dr. Carla Pontes, a scientist and healthcare researcher in South Africa.
Image: DentalProductsReport.com[/caption]
The study was conducted over a 3-month period by Dr. Shervin Molayem, a dental surgeon based in Los Angeles and founder of the UCLA Dental Research Journal, and Dr. Carla Pontes, a scientist and healthcare researcher in South Africa.
Drs. Molayem and Pontes’ study suggests that patients with bad gums are at risk of generating harmful levels of IL-6 proteins that spread to their lungs. When combined with the SARS-CoV-2 virus, it can trigger a life-threatening respiratory crisis.
Learn more about what Downtown Dental is doing to protect patient safety during the pandemic“Gum disease has been linked to other breathing ailments, including pneumonia and chronic obstructive pulmonary disease (COPD), so we weren’t surprised to find a link to respiratory problems with COVID-19,” Dr. Molayem said. “What shocked us was the discovery of the protein’s devastating, life-threatening impact to patients once they’re hospitalized. One tiny, inflammatory protein robbed them of their ability to breathe.”
READ MORE